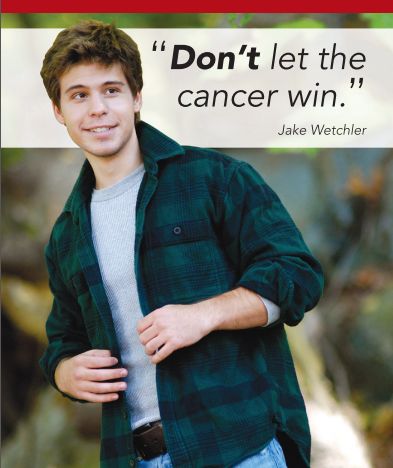
The Damon Runyon - Jake Wetchler Award
for Pediatric Innovation
Together with The Damon Runyon Cancer Research Foundation, we give a special award each year to recognize and support innovative researchers in the fight against pediatric cancer. The Damon Runyon-Jake Wetchler Award for Pediatric Innovation is given annually to a third-year Damon Runyon Fellow whose research has the greatest potential to impact the prevention, diagnosis, or treatment of one or more forms of pediatric cancer.
The Award is made in memory of Jake Wetchler, a young man who fought with indomitable spirit against two cancers. At age 18, Jake was diagnosed with Hodgkin’s lymphoma and beat the cancer into remission. But the chemotherapy he received gave him a second cancer, and with few effective treatments available, he lost his life to acute myeloid leukemia. Jake never let down in his fight against cancer, living with a powerful will and lively wit, and while cancer killed Jake, it never defeated him.
This Award in Jake’s honor recognizes scientists whose research helps to fight back against pediatric cancer, and whose innovative ideas and hard work may one day lead to cures so that young people like Jake can live their lives and fulfill their promise. This year's award is $10,000 with no restrictions on its use. The amount of the award will increase over time.
Click on the accordions below to read about how each of these researchers is working with leading edge science and technology to find better and safer treatments for children.
In September, 2025, Jon Wetchler, Beth Dominguez, Emily Levy, and I (Jean Singer) attended the Damon Runyon Cancer Research Foundation (DRCRF) Fellows Retreat, to present the annual award in Jake’s name. We were struck by the collegiality, innovative ideas, and undaunted commitment of the fellows and DRCRF staff who attended the event. The spirit of the retreat was embodied in a t-shirt that DRCRF gave to the attendees that said, “Science Saves Lives.”
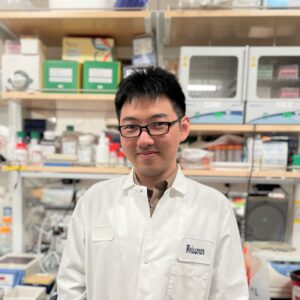
Pu Zheng, PhD
We are honored to be able to support scientists who are working to save the lives of pediatric cancer patients. This year’s award recipient, Dr. Pu Zheng, is working on a new technology that can track how cancer cells evolve over time, and using it to investigate a particularly lethal form of pediatric brain cancer, diffuse midline glioma (DMG.)
Pediatric brain tumors are among the most devastating diagnoses in childhood cancer, with DMG the deadliest of all. Children diagnosed with DMG face a median survival of less than one year, and current treatments offer only temporary relief. A major reason for this poor outcome is the tumor's extreme plasticity, or ability to shape-shift. The tumor cells constantly switch between forms that resemble different types of brain cells, making them very difficult to target.
But if we could map out how DMG cells transform over time and become therapy-resistant, we would be better able to target them or block the transitions that make them so evasive. And, if we could see where these cells take up residence in the brain and understand how certain neighborhoods create “safe havens” for transformation, we would be better able to short-circuit the mechanisms that allow DMG cells to transform.
Dr. Zheng, along with his colleagues at the Whitehead Institute, has developed just such an technology. Called the PEtracer, it installs a unique molecular “barcode” inside each cell, generating a map of how each tumor cell behaves and illuminating the pathways through which cells become therapy-resistant. This work could lay the foundation for new treatments that stop tumor cells from shape-shifting, and for diagnostics that detect dangerous cells before they are able to propagate, bringing us closer to durable and targeted therapies for some of the most urgent unmet needs in childhood cancer.
Jake believed that science saves lives. That’s why he wanted his savings to be donated to pediatric cancer research—so that scientists could find cures and other kids wouldn’t have to go through what he did. Jake was passionate about his own beliefs and would have appreciated the dedication that scientists like Dr. Zheng bring to their work. And he really would have liked the t-shirt.


More than a decade ago, cancer treatment was revolutionized by immunotherapy, a class of treatments that harness a patient’s own immune cells to fight cancer. Famously, Emily Whitehead, a 6-year-old girl with acute lymphoblastic leukemia (ALL) underwent a groundbreaking treatment called adoptive T cell therapy (ACT), which transformed her own immune T cells into a “living drug” capable of recognizing and destroying her cancer. Emily remains cancer-free today, and this innovative therapy has since provided cures for many pediatric patients with previously untreatable disease.
Despite these successes, numerous patients relapse after ACT or fail to respond to the therapy. One problem is that the therapy requires an enormous number of genetically modified T-cells – in the tens of billions – for each patient, and producing cells at this scale often involves sacrificing quality for quantity. Lower quality T-cells are less likely to persist in the patient’s body and control tumors over the long term, opening the door to relapse.
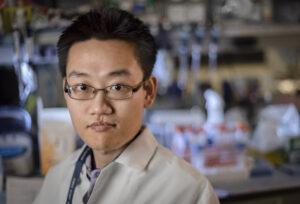
Yapeng Su, PhD
Dr. Yapeng Su has found an innovative approach to solving this problem. In his work at the Fred Hutchinson Cancer Center, Dr. Su has used powerful computational methods to determine how large quantities of high quality T-cells can be produced. He has analyzed vast amounts of data on T-cell metabolism, and has discovered that modifying the “diet” of the T-cells during production by adding a sugar called mannose, can produce large numbers of high quality cells. He has demonstrated in various tumor models that these T-cells have enhanced functionality leading to longer-term tumor control and increased survival benefits. Dr. Su’s approach holds the potential to develop “off the shelf” T-cell products with a more durable immunotherapy response, helping to reduce non-response and relapse, and making ACT more broadly available and effective for kids with cancer.
Jake fought cancer in the same way he lived his life. A philosopher at heart, he thought deeply about justice and integrity – and the greatest injustice of all was the cancer that was stealing his life. Jake did everything he could to fight and did it in his own way, with humor, strength, and style. After outpatient chemo, he had a routine: we would go out to the local Elephant and Castle restaurant for a big plate of hot chicken wings, and then he would head over to the JCC for an hour of weightlifting. It was his way of showing that cancer could not conquer his indomitable spirit.
When Jake learned that the cancer would take his life, he asked that his savings be given to cancer research so other kids wouldn’t have to go through what he did. We like to think that Jake would be pleased to see how this award in his name is helping to support scientists like Dr. Su and his promising research.
One of the greatest challenges in cancer research today is translating important discoveries from early lab studies into drugs that can be tested in patients. Nonetheless, this year’s Award recipient, Dr. Qinheng Zheng, has done just that – he has developed a molecule that acts against a cancer-causing mutation that has been well-known but difficult to target.
 In his work at the University of California, San Francisco, Dr. Zheng is focused on developing inhibitors that can suppress the action of a cancer-causing mutation called K-Ras. Scientists have known for some time that many aggressive adult cancers are driven by K-Ras mutations. After extensive research, Dr. Zheng found that a specific type of K-Ras mutation called G12D is also prevalent in pediatric cancers, such as juvenile myelomonocytic leukemia, B-cell acute lymphoblastic leukemia, and acute myelogenous leukemia. However, in contrast to the extensive studies on K-Ras in adult cancers, little research has been done on K-Ras (G12D) in childhood cancers – and there are currently no approved drugs that directly target this mutation. K-Ras is notorious for its lack of “druggability”; that is, drugs have a hard time binding to it.
In his work at the University of California, San Francisco, Dr. Zheng is focused on developing inhibitors that can suppress the action of a cancer-causing mutation called K-Ras. Scientists have known for some time that many aggressive adult cancers are driven by K-Ras mutations. After extensive research, Dr. Zheng found that a specific type of K-Ras mutation called G12D is also prevalent in pediatric cancers, such as juvenile myelomonocytic leukemia, B-cell acute lymphoblastic leukemia, and acute myelogenous leukemia. However, in contrast to the extensive studies on K-Ras in adult cancers, little research has been done on K-Ras (G12D) in childhood cancers – and there are currently no approved drugs that directly target this mutation. K-Ras is notorious for its lack of “druggability”; that is, drugs have a hard time binding to it.
Dr. Zheng has developed a first-in-class inhibitor of K-Ras(G12D) that suppresses cancer cell growth and proliferation. The lead molecule in his experiments stalled tumor growth in mouse models of pancreatic cancer while sparing cell lines without the K-Ras(G12D) mutation, suggesting that drugs developed from this technology have the potential for both efficacy and safety. Dr. Zheng’s work in this adult cancer paves the way for researchers to advance this inhibitor into preclinical and clinical trials for pediatric cancers including acute myeloid leukemia, which is the cancer that took Jake’s life.
As I (Jake's mom) do each year when presenting the the Damon-Runyon - Jake Wetchler Award, I try to give the young researchers in the room a sense for what the world loses when kids die from cancer. It is, of course, impossible to do! But I did my best to describe Jake, with his deep brown eyes that looked right at you and met your gaze, and how in Jake’s physical presence you could feel the clarity of his thoughts, the strength of his beliefs, and the warmth in his heart. I described Jake’s indomitable spirit in the face of cancer, how one time after radiation treatments, he refused to get in the wheelchair and instead wheeled his 210 pound dad merrily down the hallways. Or how, when he was diagnosed with a second cancer, acute myeloid leukemia, Jake didn’t bemoan his fate but instead decided to take up the guitar. In a hundred ways, Jake showed that whether he lived or died, he would not be defeated. With this year’s Award, we continue to raise awareness among leading-edge researchers of the impact that their work can have on the lives of young cancer patients like Jake.
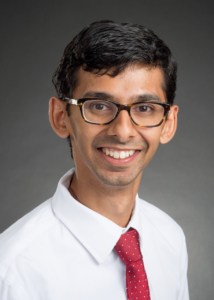
Dr. Anand Patel works at St. Jude Children's Research Hospital as a pediatric oncologist and researcher, providing care for children with cancer and investigating ways to improve their treatment options. “One of the most frustrating experiences as a pediatric oncologist is that treatment often works initially, but months or years later, the cancer comes back,” he explains. “I want to understand—why aren’t we able to get it on the first try?”
Dr. Patel’s research focuses on rhabdomyosarcoma (RMS), a fast-growing childhood cancer that can spread from muscles to other parts of the body. Despite aggressive efforts over the last 30 years to intensify therapy and develop targeted agents, outcomes for patients with metastatic RMS have failed to improve. During his pediatric oncology training, Dr. Patel was struck by the high rates of disease recurrence among children with RMS. That led him to pursue studies of how a small minority of tumor cells are able to survive chemotherapy and ultimately drive recurrence.
Dr. Patel and his collaborators have discovered that RMS tumors contain different subpopulations of cells that mimic different stages of early muscle development. Certain rare cell types are able to survive and persist through conventional treatments, and are left to divide and propagate tumors. Dr. Patel is working with a team of mathematicians and computer programmers to determine the biology of these cell subpopulations and uniquely target them. The ultimate aim of his research is to uncover novel therapeutic targets and drugs for the treatment of pediatric RMS. “It's a tremendous privilege to be a physician scientist,” Dr. Patel says. “It gives me an opportunity to bring my patients’ problems and challenges to the lab and spend the necessary time and resources to try to address their suffering.”
In this year’s award presentation, Jean Singer spoke about Jake’s indomitable spirit in the face of cancer. Jake was the kid blasting the Rocky theme song from his hospital room, and despite massive doses of chemotherapy and radiation, he never lost his strength and dignity, or the twinkle in his eye and his knack for the clever quip. We applaud Dr. Patel for the unwavering spirit that he brings to pediatric cancer research and the promise that his research holds for better treatments for kids.
Dr. Wu’s research focuses on hepatoblastoma, which is the most common childhood liver malignancy and often strikes very young children, most of whom are less than five years old. Her research has made great strides towards understanding how to shut down hepatoblastoma and offer more effective and less toxic treatments for the very young children who suffer from this form of cancer.
Hepatoblastoma researchers often hit roadblocks because of a lack of experimental models, which generally take the form of cancer cells grown in the lab that scientists can use to identify and shut down the pathways driving the disease. Dr. Wu’s research is making a big difference here. She has generated novel 3D cell lines, also called tumoroids, in which cells can grow in all three directions, as they would in the human body—unlike conventional 2D models. The 3D models/tumoroids do a much better job of mimicking cell behavior.
Importantly, using her novel tumoroid models, Dr. Wu discovered that the proliferation of hepatoblastoma depends on growth factors that act through certain cell surface receptors. She was able to halt disease growth in the lab by adding a readily-available inhibitor targeting these receptors. Dr. Wu’s research paves the way to using this inhibitor for children with hepatoblastoma.
Dr. Wu’s tumoroid models also provide a new system for scientific studies and drug screens. They hold potential for the development of personalized models that can identify the therapeutic agents expected to work best for specific patients.
In this year’s presentation of the Award at the Damon Runyon Fellow's Symposium, Jake's dad, Jon Wetchler, spoke about Jake’s fight against acute myeloid leukemia, a cancer for which there were not many safe or effective treatments. Jon described how Jake responded to the knowledge that there was little out there to save his life. Since he couldn’t control whether he lived or died, Jake decided to focus on what he did hold in his power, and set two goals for himself:
1. Going the distance. He would use all of his logic, all of his strength, and all of his heart to do whatever he could to make it to a stem cell transplant.
2. Not to let cancer win. He made up his mind that he would not let cancer steal his soul by taking away who he was or controlling what he felt or did.
Jake more than went the distance because he fought his fight to the end, on his own terms. And although he died, he was never defeated.
When Jon told Jake’s story to the Damon Runyon researchers—who are engaged in their own fight against cancer in the laboratory—he showed them a picture of a board Jake split during one of his karate tests, and that hangs on the wall of his room in our house. This board was a particularly tough one for him to break, but after he finally did, he mounted it and wrote this message:

We are grateful to Dr. Wu and all the Damon Runyon researchers for their perseverance in the fight against pediatric cancer.

Dian Yang, PhD, is working at the Whitehead Institute for Biomedical Research, pioneering new technologies to better understand the complicated make-up of tumors and how they evolve to metastasize and become therapy-resistant. He has developed an innovative "molecular recorder" that allows scientists to trace tumor evolution at unprecedented resolution in pediatric and adult cancers. Uncovering how individual tumor cells evolve and spread through the body has the potential to guide better drug development.
Dr. Yang is applying this novel technology to osteosarcoma, the most common form of bone cancer in children, teens and young adults. Osteosarcoma is highly aggressive and metastatic, and the 5-year survival rate is below 30% in late stage patients. Despite efforts over the past 35 years, therapies for this deadly cancer have not improved. "By analyzing how the genes in individual cancer cells change and evolve, we aim to identify new diagnostic markers and potential therapeutic targets," said Dr. Yang
"I was struck by Dian's strategy of using cutting-edge technology to get better treatments to children and young adults - such a challenging disease will take true innovation to make progress," said Beth Dominguez, our Director of Scientific Affairs.
Dr. Yang entered pediatric cancer research as a graduate student at Stanford. "My neighboring lab worked on pediatric cancers. I heard some heartbreaking patient stories, and I learned a great deal about the challenges. This motivated me to apply our technologies to pediatric patient samples which may behave differently than adult tumors," explained Dr Yang.
Jon Wetchler presented this year's award. He talked about Jake's courageous fight against cancer and the role that passion and heart can play in scientific breakthroughs. He encouraged scientists to follow research and discovery that comes from the heart, in the spirit of helping children and young adults with cancer.
When accepting the award, Dr. Yang insisted, "This award is not just for me but for all the pediatric researchers because each of us contributes a little and then together we contribute a lot." We continue to be inspired by the exceptional researchers we find in the fight against pediatric cancer.
 At the age of 14, Marissa Rashkovan decided that her mission in life would be to cure cancer. Her mother had been diagnosed with Stage 3 Follicular B cell lymphoma, and Marissa watched as she battled through harsh chemotherapy and a stem cell transplant, only to see the cancer come back in another, more aggressive form. More intense chemotherapy followed, along with a second stem cell transplant. Thankfully, today, 15 years later, Marissa’s mother is cancer-free. Her illness, however, had a profound effect on Marissa’s family and herself, and led to Marissa’s commitment to becoming a cancer researcher.
At the age of 14, Marissa Rashkovan decided that her mission in life would be to cure cancer. Her mother had been diagnosed with Stage 3 Follicular B cell lymphoma, and Marissa watched as she battled through harsh chemotherapy and a stem cell transplant, only to see the cancer come back in another, more aggressive form. More intense chemotherapy followed, along with a second stem cell transplant. Thankfully, today, 15 years later, Marissa’s mother is cancer-free. Her illness, however, had a profound effect on Marissa’s family and herself, and led to Marissa’s commitment to becoming a cancer researcher.
Marissa Rashkovan, PhD, now works at Columbia University, where she is studying a highly aggressive form of blood cancer called ETP acute lymphoblastic leukemia (ETP-ALL.) This disease is notoriously difficult to treat, with survival rates around 13%, and children who do survive face significant side effects later in life from the intense chemotherapy regimens.
Dr. Rashkovan has found a unique metabolic pathway in ETP-ALL that can be targeted for treatment -- and potentially with already-known drugs on the market. She is screening FDA-approved drugs to find candidates that may act on ETP-ALL cancer cells, an approach that takes advantage of compounds with already-established safety profiles, and that could speed new treatments to patients greatly in need. Her innovative approach is advancing important science and holds promise for better and safer treatments for a high-risk pediatric cancer.
Dr. Challice Bonifant is working to revolutionize cancer treatments for children by engineering cells from the patient’s own immune system so they can recognize and kill the cancer. Her research focuses on acute myeloid leukemia (AML), which is the disease that took Jake’s life and is a devastating form of cancer with high levels of treatment-related toxicity and low survival rates.
While immunotherapy treatments have been successful with other types of leukemia, such as Acute Lymphocytic Leukemia (ALL), AML is more difficult to attack because the target proteins found on malignant cells are also found on normal cells. Targeting these would therefore cause toxicity to the normal cells - an unacceptable side effect. Dr. Bonifant has taken the innovative approach of designing T immune cells that can target two proteins at the same time. This dual expression is common for disease cells but rare in healthy ones, enabling the treatment to more precisely kill the cancer cells. Tests in animal models have shown promise and Dr. Bonifant has filed for a provisional patent, with the intent that her work lead to the development of a clinical therapy for pediatric AML.
Both a researcher and a pediatrician, Dr. Bonifant is driven by a powerful desire to see breakthroughs from her lab impact patient lives. This passion for translating discoveries into treatments started when she was an undergraduate researcher at Wake Forest University, working on the biochemical mechanism of hydroxyurea metabolism, for treating sickle cell disease. At the time, she was also volunteering in the local children’s hospital and happened to serve dinner to a teenage girl with sickle cell disease. The girl was excited to have begun taking a new medication with much promise for turning her disease around. The medicine was hydroxyurea. For Dr. Bonifant, the connection between laboratory investigation and the relief of human suffering was made.
In January, 2019, Dr. Bonifant will be moving from her current position at the University of Michigan to the Bloomberg-Kimmel Institute for Cancer Immunotherapy at Johns Hopkins. The institute was established as a part of the Cancer Moonshot initiative, with the express purpose of accelerating the movement of discoveries from the lab to patients in need.
In Dr. Bonifant’s words, “Working with pediatric patients and in particular pediatric patients who are suffering either from their cancer or from the toxicity of their cancer treatment is what motivates me every day in the lab to try to do better, to work harder, and to find a solution.”
Dr. Amanda Balboni Iniguez had a passion for science from a very young age and was inspired to become a cancer biologist in high school, when she became involved in the American Cancer Society’s Relay for Life fundraiser. “Hearing stories from cancer survivors motivated me to pursue a career as a cancer scientist,” she says. “My ultimate goal is to develop new therapies that will improve survival with decreased side effects for pediatric patients.”
Her current research focus is on a class of compounds to treat pediatric neuroblastoma, a devastating cancer that most commonly affects children age five years or younger. Neuroblastoma typically forms in immature nerve cells resulting in tumor growth in the neck, chest, abdomen, or spine of the child. Currently, there are few effective treatments for neuroblastoma, and the disease accounts for 15% of all childhood cancer deaths.
Dr. Balboni Iniguez is targeting epigenetic regulators in cells as an innovative approach to shutting down the disease. These regulators act as the on/off switches controlling the production of proteins. In cancer cells, the switches often malfunction, allowing the cells to grow out of control. Dr. Balboni Iniguez's work has profound implications for the clinical treatment of high-risk neuroblastoma and may offer an effective treatment strategy for patients with advanced disease. Her discoveries in this field may translate into treatments for other cancers as well.
Dr. Balboni Iniguez's work in neuroblastoma builds on her research accomplishments in another pediatric cancer, Ewing sarcoma, which is a rare solid tumor of the bone or tissue surrounding the bone that strikes children and young adults. This research selectively targeted a protein driving the disease and identified a molecule that inhibits its progression, offering an opportunity for clinical treatments. Her discovery also increases our understanding of this childhood cancer’s cell biology, and has been submitted to the prestigious journal, Cancer Cell, for publication.
“It was a huge surprise to me to win the Jake Wetchler Award for Pediatric Innovation." says Dr. Balboni Iniguez. "...it is encouraging any time you receive recognition for your work, however, this is particularly special for me. It was an honor to meet the founders of the Jake Wetchler Foundation, who have bravely championed for innovative research in the field of pediatric oncology and are very familiar with the unique challenges this field faces... I continue to dedicate my life to understanding some of the most devastating pediatric cancers and I hope to make a real difference in the lives of children affected with these diseases.”
Dr. Zimmerman’s research focuses on neuroblastoma, a particularly devastating cancer that strikes very young children. The median age of these cancer patients is just seventeen months – they are infants, toddlers, and grade school children. High risk neuroblastoma has few effective treatments, and the disease accounts for 15% of all childhood cancer deaths.
Dr. Zimmerman’s interest in cancer began as a biochemistry student at the Rochester Institute of Technology where he became fascinated with the mechanisms by which normal cells become malignant. Later, during his post-doctoral work at Dana-Farber Cancer Institute, he visited the Jimmy Fund Clinic where children were undergoing chemotherapy, and was deeply moved by the need for research into better pediatric treatments. As a result, he decided to focus his post-doctoral efforts on pediatric oncology.
Dr. Zimmerman’s current project, Elucidating the mechanism of CHD5-mediated tumor suppression in neuroblastoma, seeks to understand the function of a particular family of genes, called the MYC oncogenes, that have been found to play a role in malignancy. MYC functions as a master regulatory gene, working in concert with various enzymes and transcription factors to direct gene expression. Dr. Zimmerman has already identified how an insufficiency of the enzyme CHD5 accelerates tumor growth in a zebrafish model of neuroblastoma by enabling MYC to overcome rate-limiting constraints on cell proliferation. Using a combination of innovative computational and biochemical methods, he is now defining and validating the core transcriptional unit essential for neuroblastoma cell survival and the transcriptional circuitry that emerges from it. With this knowledge, we may ultimately be able to develop targeted therapeutics to shut down the circuits necessary for the cancer to grow.
We are fortunate to have as our first award recipient such a gifted scientist who is also dedicated to saving the lives of children with cancer.
